Vasectomy is a safe, effective, and permanent method of contraception. It should be considered in men who wish for:

What is a Vasectomy?
Sperm are produced in the testicles before moving into the epididymis, which sits on the back surface of each testicle. These sperm remain in the epididymis where they mature. The sperm then travels up each vas and are expelled at the time of ejaculation in the semen.
When a vasectomy is performed, the vas deferens are cut and sealed, preventing sperm from leaving the epididymis. This way, no sperm are expelled from the penis at the time of ejaculation.
If you would like more specific information on Vasectomy please view one of the following pages. If what you are looking for is not there, please don’t hesitate to give us a call today. We are more than happy to help you & educate you.
Vasectomy success rates
Vasectomy is successful in more than 99 percent of men. Other methods of contraception are required until a semen analysis confirms there are no sperm in the semen.
The sperm count is checked approximately three months after the procedure. A man needs to have had at least 20 ejaculations after vasectomy to clear the ducts of sperm.
If the semen analysis shows sperm that do not move there is a small chance that a pregnancy may occur. Other methods of contraception should be continued until a clear test result is completed
Vasectomy Procedure
Men who are considering a vasectomy have a consultation before the procedure. At this appointment, the doctor will explain the procedure and answer any questions.
Vasectomies can be performed under a local or general anaesthetic. There will be a small scar from the incision but this will not be very noticeable once it has healed.
After the Procedure
You may go home shortly after your procedure. Preferably someone else should drive you home.
Pain control following Vasectomy
After the vasectomy, there may be some discomfort at the incision site. This can be relieved with a pain medication such as paracetamol. Ibuprofen and aspirin should be avoided for at least one week to minimise the risk of bruising and bleeding around the incision.
Semen tests
You are not clear to discontinue the use of other forms of contraception until you have been formally advised that you have achieved a zero sperm count at least three months and a minimum of 20 ejaculations following surgery.
Health effects of Vasectomy
Sex drive
Having a vasectomy will not affect testosterone levels, sex drive, or the ability to have an erection.
Risk of cancer
Although there have been some concerns regarding a link between vasectomy and prostate and testicular cancer, several large studies suggest that there is no increased risk of any cancer. Heart disease – similar to the situation with cancer, despite some concerns, studies have not found any link between vasectomy and heart disease.
Contraception after a vasectomy
If the semen analysis shows no evidence of sperm you may discontinue the use of other forms of contraception. Vasectomy does not protect against sexually transmitted diseases such as HIV.
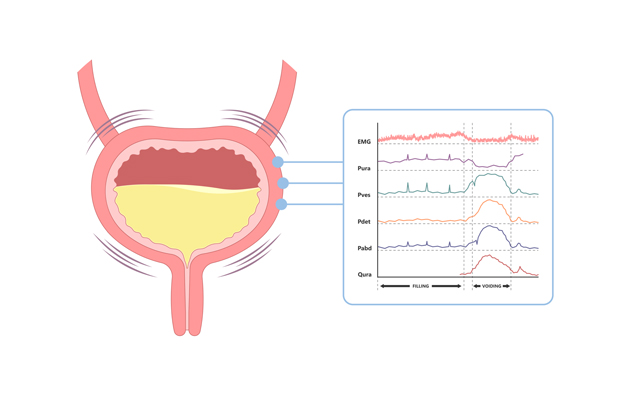
Urodynamic testing is often used to try and find out what is causing bladder problems. It is the study of the bladder’s ability to hold and empty urine. It measures the way the bladder relaxes to fill and then contracts to empty. The evaluation is assisted with a computerised study.
Allow a total appointment time of one and a half hours for test and review by the doctor.
Before the Procedure
During the Procedure
After The Procedure
A prostate biopsy is a safe and effective sampling technique during which tissue is obtained from the prostate gland for the purpose of detecting cancer.
Trans rectal ultrasound guided biopsy is the preferred approach in most cases. It involves the examination of the prostate by an ultrasound probe inserted into the rectum. After local anaesthetic has been injected, a fine needle is inserted into the prostate and a number of small samples (biopsies) are taken.
Allow a total appointment time of 30 minutes, although the procedure itself normally takes 5-10 minutes.

Before the procedure
During the procedure
After the procedure
Risks and complications
Infection
If you feel unwell with a headache, sweating, fevers, chills, painful testicles or problems passing urine, you need to contact your Urologist immediately as you may require admission to hospital for further treatment.
Bleeding
You may experience blood in your urine, bowel motion and semen and this will gradually subside over the next 2 weeks and rarely causes a problem. If bleeding persists or is very heavy, contact your doctor.
Inability to urinate
This can occur due to swelling around the prostate and may rarely lead to a complete blockage of urine flow. If this occurs, contact your doctor.
Pain and discomfort
You may experience discomfort in the rectum or base of the penis. This is very common and should settle within 24-48 hours.
What is Laparoscopic surgery?
Laparoscopic surgery (‘keyhole’ or ‘minimally invasive’ surgery) is the technique of performing surgery through multiple small incisions, rather than one large incision Through these small incisions, ‘ports’ are placed to pass a telescope, light source, and instruments, and carbon dioxide is used to inflate an operating ‘workspace’.

Advantages
Disadvantages
What is a laparoscopic nephrectomy?
This procedure involves removing the kidney through ‘key hole’ surgery. The procedure is most commonly performed to remove cancer but may be indicated to remove a kidney severely damaged by obstruction, stones, or infection. The procedure is performed through 3 or 4 incisions in the front of the abdomen, or the back, depending on specific technique used. If the kidney is removed for cancer, one incision is enlarged to 6 – 8 cm to allow removal of the kidney intact for further analysis. If it is too difficult to complete the surgery laparoscopically, a larger cut is made to remove the kidney through more traditional open surgery. This is necessary in around 5% of cases.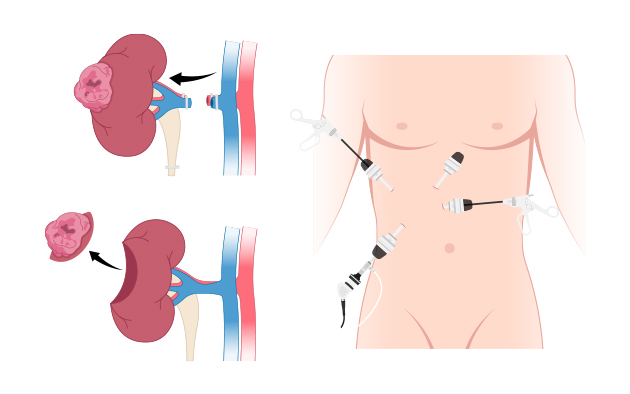
How long does it take?
3-4 hours under a general anaestheticWhat are the risks?
What can I expect after surgery?
Living with one kidney
One kidney can easily support a normal and active life. There is no need to limit activities or lifestyle.
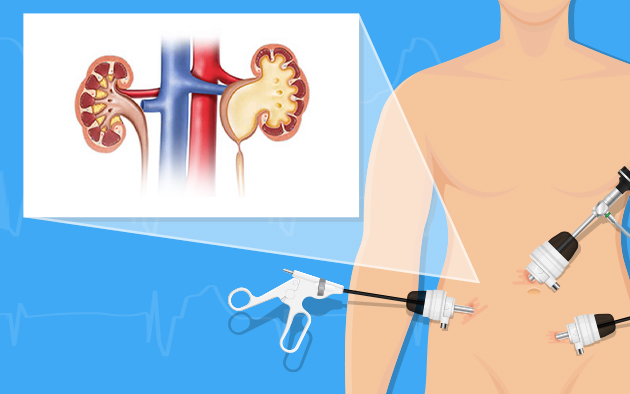
What is a laparoscopic pyeloplasty?
This is an operation to remove the blockage between the outlet of the kidney (renal pelvis) and the kidney tube (ureter). This condition is called pelvi-ureteric junction (PUJ) obstruction. This blockage is mostly due to a blockage that occurs from birth, due to abnormal development of the kidney. Rarely it can be due to the previous scarring that narrows the tube, caused by stones, trauma or previous surgery.
Key-hole surgery is performed through 3 – 4 incisions through the side of the abdomen to remove the blockage. A small tube (stent) is left in the ureter for 4-6 weeks to allow the tube to heal. This is then removed under local anaesthetic by passing a small telescope (cystoscope) into the bladder.
Conversion to a conventional open operation can occur if the procedure can not be performed through key-hole surgery. This occurs in approximately 5% of cases.
Why do I need this?
The operation is needed if the blockage causes kidney pain, kidney infections or the kidney function becomes damaged. It can also be associated with kidney stones and high blood pressure.
How long does it take?
4-5 hours under a general anaesthetic
What are the risks?
What can I expect after surgery?
What is Ureteroscopy?
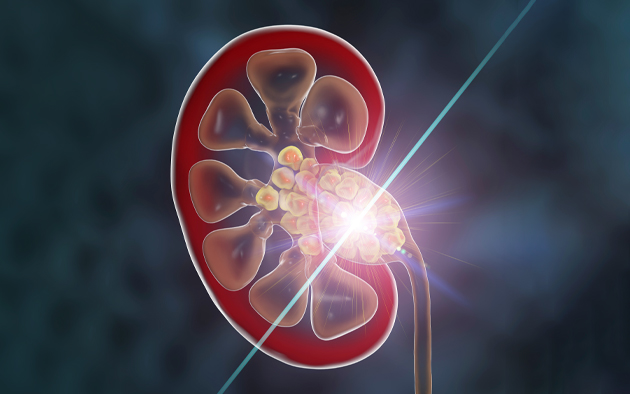
Why do I need this?
You have a stone in your ureter, less than 2 cm in size, which may be causing pain, obstruction, bleeding or infection
How long does it take?
30 – 60 minutes under a general anesthetic, depending on the stone size, location, and hardness
What are the risks?
What can I expect after surgery?
The following day, any catheter if placed, is removed and you can go home once you have passed urine
What is TURBT?
Why do I need this?
To remove a bladder tumor and determine if it is a cancer and its extent
How long does it take?
20 – 40 minutes under a general anaesthetic
What are the risks?
What can I expect after surgery?
Bladder Cancer Patient Guidebook
Canadian Patient Guidebooks – Downloads – Bladder Cancerhttps://bladdercancercanada.org › canadian-patient-guide
What is a ‘TURP’?

How long does it take?
What do I need to do before surgery?
What are the risks?
What can I expect after surgery?
Holmium Laser Enucleation of the prostate (HoLEP) is a modern alternative to the standard Transurethral Resection of the Prostate (TURP) procedure for bladder outflow obstruction due to BPH. It requires a short period of hospitalisation and a general anaesthetic. A catheter (a tube which drains the bladder) is required for 1-2 days until the urine is clear. Patients are advised to take life quietly and to avoid straining or heavy lifting for four weeks after the surgery.

Who is it suitable for?
What does the procedure involve?
A laser is used to help remove tissue from the prostate gland which is causing a restriction to the flow of urine out of the bladder.
What are the advantages of HoLEP?
What problems can occur after surgery?
Common (greater than 1 in 10)
• Temporary burning, bleeding and frequency of urination
• No semen produced with orgasm (75 out of 100 men) – permanent
• Not all urinary symptoms may resolve
• Infection of bladder, testes or kidneys
• Failure to pass urine requiring temporary catheter placement
Occasional side-effects (1 in 10 to 1 in 50)
• Loss of urinary control
• Damage to erections
• Injury to urethra (water-pipe) causing scarring, further operation may be required
• Finding of unsuspected cancer in the tissue removed from the prostate
Rare side-effects (less than 1 in 50)
• Repeated treatment for re-growth of prostate gland (1% at seven years)
• Self-catheterisation or indwelling catheter if bladder is weak
• Ongoing loss of urinary control (incontinence), further operation may be required (less than 1%)
• Retained tissue fragments in bladder, may require telescopic procedure
• Injury to ureter (drainage tube from kidney)
• Perforation of bladder needing further surgery
• Bleeding requiring return to operating theatre
Your Urologist will be happy to discuss HoLEP with you.
What is an insertion of penile implant?
Why do I need this?
This procedure is reserved for severe erectile dysfunction where sexual intercourse is not possible and other treatments have failed or are unsuitable
How long does it take?
90 – 120 minutes under a general anaestheticWhat are the risks?
What can I expect after surgery?
ZSR Stapler Circumcision
Circumcision surgery is the surgical removal of the penile foreskin for various medical reasons (infection, balanitis, BXO, penile cancer, STD prevention). It is also performed for religious or cosmetic reasons to have a cleaner appearance of the male genital.
Circumcision reduces the risk of contracting UTIs, STIs, HIV, etc. It can even lead to lower risk of developing penile cancer in men and cervical cancer in their sexual partners.

What is Stapler Circumcision?
Stapler circumcision is a minimally invasive technique to perform circumcision that is used for safe, quick and efficient removal of the penile foreskin. The procedure is performed using a circumcision stapler (also called anastomat), an instrument specially designed for circumcision.
Stapler Circumcision Procedure
During the procedure, a local anaesthetic is administered at the base and shaft of the penis. This ensures safe and effective pain relief during the surgery and minimises post-operative pain for several hours.
Thereafter, the stapler is fitted over the penis, and once fired, it removes the foreskin in one quick motion and closes the incision using a silicone ring/non-bioabsorbable staples. Since the amount of foreskin to be removed is predetermined in the procedure, it is extremely safe and provides the desired results for both the patient and the surgeon.
Recovery and Healing Tips
Stapler Circumcision – Benefits & Side Effects
Stapler circumcision is an advanced circumcision procedure that allows for faster recovery and better results as compared to open circumcision.
The downside of stapler circumcision is the delay in extrusion of staples that may happen in some cases but in routine surgical circumcision the sutures take time to fall off as well.
Some cases depending on the penile anatomy may not be suitable for stapler circumcision and surgical circumcision is advised in these cases.
 +973 66907199
+973 66907199