When you think of testosterone, what comes to mind? Macho men? Aggressive, impatient, type A behavior? Road rage? Violence? Testosterone’s role in bad behavior is largely a myth. What’s more, testosterone plays other important roles in health and disease. Testosterone is a key player in Prostate cancer. Women need testosterone too.
Contents
- 1 Testosterone: What it does and what it doesn’t do
- 2 Testosterone plays several important roles in males:
- 3 Does women have testosterone?
- 4 Did you know?
- 5 Testosterone levels at different ages
- 6 Normal Testosterone Levels
- 7 Problems associated with abnormally high testosterone levels in men include:
- 8 High Testosterone and Risk Of Metabolic Disorders and Cancers
- 9 Did you know?
- 10 Natural Ways To Boost Your Testosterone
- 11 A. Boost Testosterone with Exercise
- 12 B. Boost Testosterone with Nutrition
- 13 C. Boost Testosterone with Supplements
- 14 D. Lifestyle Strategies for Increased Testosterone.
- 15 Low Testosterone
- 16 Causes Of Low Testosterone
- 17 How Common is Low Testosterone (Low-T) in Men?
- 18 Can low testosterone be prevented?
- 19 Did you know?
- 20 Male Aging/ Andropause / Androgen deficiency in aging male/ Late-onset hypogonadism
- 21 History of Male Menopause
- 22 What are the symptoms of low testosterone?
- 23 How is low testosterone (Low-T) diagnosed?
- 24 How is low testosterone treated?
- 25 What are the benefits of TRT?
- 26 What are the side effects of TRT?
- 27 Prostate Cancer Risk and Testosterone Replacement
- 28 Who shouldn’t take testosterone replacement therapy?
- 29 Did you know?
Testosterone: What it does and what it doesn’t do
Testosterone is the major sex hormone in males. It is produced by testis. Signals sent from the brain to the pituitary gland at the base of the brain control the production of testosterone in men. The pituitary gland then relays signals to the testes to produce testosterone. A “feedback loop” closely regulates the amount of hormone in the blood. When testosterone levels rise too high, the brain sends signals to the pituitary to reduce production.
Testosterone plays several important roles in males:

Does women have testosterone?
Testosterone also plays important role in females. Testosterone is produced in the ovaries and adrenal gland in females. These hormones are thought to have important effects on:
- Ovarian function
- Bone strength
- Sexual behavior, including normal libido (although evidence is not conclusive)
The proper balance between testosterone (along with other androgens) and estrogen is important for the ovaries to work normally. While the specifics are uncertain, it’s possible that androgens also play an important role in normal brain function (including mood, sex drive and cognitive function).
Did you know?
Testosterone is synthesized in the body from cholesterol. But having high cholesterol doesn’t mean your testosterone will be high. Testosterone levels are too carefully controlled by the pituitary gland in the brain for that to occur.
Testosterone levels at different ages
Testosterone levels are at their highest during adolescence and early adulthood. In boys, the first physical signs of testosterone, or androgens, in the body are apparent during puberty. A boy’s voice changes, his shoulders broaden, and his facial structure becomes more masculine. As men get older, their testosterone levels may decline about 1 percent per year after age 30.
Normal Testosterone Levels
The “normal” or healthy level of testosterone in the bloodstream varies widely, depending on thyroid function, protein status, and other factors. According to recent guidelines from the American Urological Association (AUA), a testosterone level of at least 300 nanograms per deciliter (ng/dL) is normal for a man. A man with a testosterone level below 300 ng/dL should be diagnosed with low testosterone.

‘The higher the testosterone the lower the maturity level…’ – Jenifer DeCuir, Wynter’s Journey
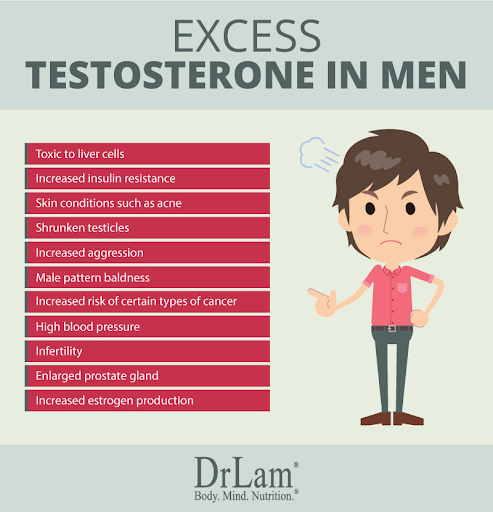
Excess testosterone in men can result from testicular or adrenal tumors. These tumors can be non-cancerous, yet still boost testosterone levels to unhealthy levels, as can steroid use and testosterone abuse. Some men actually have a genetic predisposition for developing high levels of testosterone. These men are at a much higher risk for developing blood clots, heart disease, and a variety of other cardiovascular issues.
Problems associated with abnormally high testosterone levels in men include:
High Testosterone and Risk Of Metabolic Disorders and Cancers

It is essential that men with high testosterone are tested and are aware of their potential risks.
Did you know?
Women can have high testosterone levels.
Among women, perhaps the most common cause of a high testosterone level is polycystic ovary syndrome (PCOS). This disease is common. It affects 6% to 10% of premenopausal women.
Natural Ways To Boost Your Testosterone
TESTOSTERONE IS THE CRUCIAL MALE HORMONE IN THE HUMAN BODY. UNDERSTANDING ITS EFFECTS AND KNOWING HOW TO BOOST ITS LEVELS HELPS BOOST PHYSICAL FITNESS.
If you want to boost your natural testosterone levels, it helps to know all the best strategies — both in and out of the gym.
A. Boost Testosterone with Exercise
“Training to build muscle mass elevates testosterone, and elevated testosterone helps build muscle mass.” Just make sure you don’t do too much. When you overdo weight training and go past the point, instead of elevating testosterone, you boost stressful cortisol levels, which can reduce your muscle mass and testosterone levels. To maximize testosterone levels, include the following exercise strategies.
1. Train smart with weights
Keep hardcore weight-training sessions to 4–5 per week, and finish workouts in 60–75 minutes. Emphasize sets that max out at 5–8 reps, and reduce rest periods to about two minutes between sets to include more sets in a shorter time span.
2. Keep your cardio moderate.
Perform moderately paced cardio such as an easy jog or fast-paced walk on a treadmill. Sessions should not be longer than 30–45 minutes, and no more than about four a week, especially when you’re trying to add muscle mass.
B. Boost Testosterone with Nutrition
Certain dietary adjustments help you naturally boost your testosterone levels.
1. Consume plenty of protein.
Consume at least 1 gram of protein for each pound of your bodyweight every day, and strive to get in about 30% of your total calories from protein each day.
2. Consume cruciferous vegetables.
“Research has shown that consuming a diet rich in cruciferous vegetables such as broccoli, cabbage, brussels sprouts, collards, watercress, kale, kohlrabi, mustard greens and bok choy may help boost testosterone levels.” This is due to the phytonutrients they contain, including indoles, which help suppress estrogen.
3. Eat plenty of fats.
Saturated fats, which are considered “unhealthy”, provide the raw materials your body needs to produce hormones such as testosterone. 10% of your daily calories may be consumed in the form of saturated fats. In addition, 10% of your daily calories should be from unsaturated fat sources such as oils (olive and canola) and fatty fish (salmon. In total, dietary fat should constitute 20% of total caloric intake.
4. Grapes
Grapes contain many vitamins that contribute to overall health. Chinese researchers have found that 5-10 g of grape skins improves sperm motility and increases testosterone levels.
5. Avoid alcohol.
Keep alcohol consumption to no more than 1–2 drinks per day.
6. Other food items that boost Testosterone.
Egg yolk, beef, shell fish, fatty fish, tuna, oysters, extra virgin olive oil, pomegranates, fortified plant milks, onions, green leafy vegetabes, garlic, beans are some other food items that may naturally boost testosterone production.
C. Boost Testosterone with Supplements
Certain supplements taken daily like cordyceps (from mushrooms, 300-450mg), Tribulus terrestris (from a herb growing North America and Asia, 500-2000 mg), fenugreek (500-600mg), ginseng (40-50mg twice a day) can help in boosting testosterone levels naturally. 30 mg per day of Zinc supplements showed an increase in free testosterone levels
D. Lifestyle Strategies for Increased Testosterone.
1. Get plenty of sleep.
Get at least 7–8 hours of sleep per night, striving for the high end on days when you train harder such as when doing legs or back.
2. Schedule days off from the gym.
At least once a week give your body a full day of recovery with no weights, cardio or any other stressful forms of activity.
3. Have sex regularly.
With a partner or alone, frequent ejaculation boosts testosterone levels, which in turn works your endocrine system, helping to keep it primed.
Low Testosterone
‘When I was in my 20s I went through my testosterone phase and had a Mercedes to show that I’m rich, and they used to call me ‘Jaguar John.’ I’m older now, and I’m concerned about the environment and… appreciate a car that doesn’t pollute.’
– John Densmore
Low testosterone (male hypogonadism) is a condition in which the testes (testicles, the male reproductive glands) do not produce enough testosterone.
Causes Of Low Testosterone
Common causes include:
Some persons are born with conditions that cause Testosterone Deficiency (TD) such as:
- Klinefelter syndrome
- Noonan syndrome
- Ambiguous genitalia (when the sex organs develop in ways that are not typical looking)
Some men may develop Low-T because of conditions like these:
- Damage to testicles by accident
- Removal of testicles because of cancer
- Chemotherapy or radiation
- Pituitary gland disease leading to hormone deficiency
- Infection
- Autoimmune disease (when the body makes antibodies that attack its own cells)
Basically, if your testicles keep making less testosterone than normal, your blood levels of testosterone will fall. Many men who develop TD have Low-T levels linked to:
- Aging
- Obesity
- Metabolic syndrome (high blood pressure, high blood sugar, unhealthy cholesterol levels, and belly fat)
- Use of medications such as antidepressants and narcotic pain medications
Men with certain health problems also tend to have low testosterone. Some of these are:
- HIV (about 30 out of 100 also have low testosterone)
- AIDS (about 50 out of 100 also have low testosterone)
How Common is Low Testosterone (Low-T) in Men?
It is hard to know how many men among us have Low-T, although data suggest that overall about 2.1% (about 2 men in every 100) may have Low-T. As few as 1% of younger men may have TD, while as many as 50% of men over 80 years old may have Low-T.
Low-T is more common in men who have diabetes or who are overweight. In one research study, 30% of overweight men had Low-T, compared to only 6.4% of those with normal weight. The same study found diabetes to be a risk factor for Low T. In another study, 24.5% of men with diabetes had Low-T, compared to 12.6% of those without diabetes.
Can low testosterone be prevented?
There are no known ways to prevent low testosterone that is caused by genetic conditions or damage to the testes or pituitary gland.
A healthy lifestyle that includes good nutrition, exercise, weight management, and that avoids excessive use of alcohol and drugs can help keep testosterone levels normal.
Did you know?
Not all patients who are found to have low testosterone need to be treated.
For more details on Low Testosterone… please read the section “Male Aging”
Male Aging/ Andropause / Androgen deficiency in aging male/ Late-onset hypogonadism
What is Andropause?
“Andras” in Greek means human male and “pause” in Greek a cessation; so literally “andropause” is defined as a syndrome associated with a decrease in sexual satisfaction or a decline in a feeling of general well-being with low levels of testosterone in older man.
It is a common disorder, affects an estimated 1 in 200 men.
History of Male Menopause
Testosterone deficiency was originally conceptualized in the Talmud and Old Testament. A 16th century medical text found in China listed symptoms relating to the ideology of the male menopause syndrome. In 1944, Heller and Myers wrote what was considered a milestone paper in understanding the reversal of testosterone deficiency by testosterone replacement.
What are the symptoms of low testosterone?
Symptoms of low testosterone depend on the age of person, and include the following:
- Low sex drive
- Erectile dysfunction
- Decreased sense of well-being
- Depressed mood
- Difficulties with concentration and memory
- Fatigue
- Moodiness and irritability
- Loss of muscular strength
Other changes that occur with low testosterone include:
- A decrease in hemoglobin and mild anemia
- A decrease in body hair
- Thinning of the bones (osteoporosis)
- Increased body fat
- Breast development (gynecomastia)
- Infertility
How is low testosterone (Low-T) diagnosed?
To make a diagnosis, your doctor will assess specific signs and symptoms in addition to your testosterone blood level. It may take several measurements to determine if a patient has Low-T, since levels tend to change throughout the day. The highest levels of testosterone are generally in the morning, near 8 a.m. This is why doctors prefer to measure testosterone levels in the early morning.
Additional tests that may be advised based on your clinician’s assessment include
- Blood tests : LH (Luteinising Hormone), FSH (Follicle Stimulating Hormone), Estradiol, Prolactin, Hemoglobin, HbA1C, Free Testosterone, SHBG (Serum Hormone Binding Globulin)
- MRI (magnetic resonance imaging) of pituitary gland (located in brain)
- Bone density tests
- Karyotype (Chromosome tests)
How is low testosterone treated?
The AUA (American Urology Associaion) recommends that Testosterone Replacement Therapy (TRT) be prescribed only to men who meet the clinical and laboratory definition of testosterone deficiency (Testosterone level of less than 300 ng/dL).
TRT can be given in five different ways:
- Transdermal (Topical). There are topical gels, creams, liquids and patches. Topical medicines most often last for about four days. They absorb better if covered with an air- or water- tight dressing. A topical patch is like a band-aid with medicine on it. You put it on and leave it until the next dose is due. The medicine on the patch is less likely than liquids, gels and creams to transfer to others.
- Injection. There are short-acting and long-acting forms of testosterone injection. The short-acting medicine may be given under the skin or in the muscle. The long-acting one is usually given in the muscle. Injections are usually given either weekly, every two weeks, or monthly.
- Oral/buccal (by mouth). The buccal dose comes in a patch that you place above your incisor (canine or “eyetooth”). The medication looks like a tablet but you should not chew or swallow it. The drug is released over 12 hours. This method has fewer harmful side effects on the liver than if the drug is swallowed, but it may cause headaches or cause irritation where you place it.
- Intranasal. This form of testosterone comes in a gel. You pump the dose into each nostril, as directed. It is usually taken three times daily.
- Pellets. Your doctor will place the testosterone pellets under the skin of your upper hip or buttocks – using local anesthesia to numb your skin, a small cut is made and the pellets are placed inside the fatty tissues underneath your skin. This medication dissolves slowly and is released over about 3-6 months, depending on the number of pellets.
Talk about the choices with your doctor.
What are the benefits of TRT?
Potential benefits of testosterone replacement therapy may include:
- In boys, avoiding problems related to delayed puberty
- Loss of fat
- Increased bone density and protection against osteoporosis
- Improved mood and sense of well-being
- Improved sexual function
- Improved mental sharpness
- Greater muscle strength and physical performance
What are the side effects of TRT?
The side effects of TRT include:
- Acne or oily skin
- Swelling in the ankles caused by mild fluid retention
- Stimulation of the prostate, which can cause urination symptoms such as difficulty urinating
- Breast enlargement or tenderness
- Worsening of sleep apnea (a sleep disorder that results in frequent nighttime awakenings and daytime sleepiness)
- Smaller testicles
- Skin irritation (in patients receiving topical testosterone replacement)
Laboratory abnormalities that can occur with testosterone replacement include:
- Increase in prostate-specific antigen (PSA)
- Increase in red blood cell count
- Decrease in sperm count, producing infertility (inability to have children), which is especially important in younger men who desire fertility
If you are taking hormone replacement therapy, regular follow-up appointments with your physician are important.
Prostate Cancer Risk and Testosterone Replacement
Guidelines suggest discussing the potential risk vs. benefit of evaluating prostate cancer risk and prostate monitoring. The doctor and patient will decide together regarding prostate cancer monitoring. For patients who choose monitoring, clinicians should assess prostate cancer risk before starting testosterone treatment, and 3 to 12 months after starting testosterone:
- PSA levels should be checked at 3, 6, and 12 months within the first year, and then every year after that.
- A digital rectal examination of the prostate should be done at 3-6 months and 1 year after beginning therapy, and then every year after that. This is recommended even for men who are not on testosterone replacement therapy, as an age-related prostate cancer screening. This usually begins at age 50.
- Hematocrit levels will be checked before testosterone therapy starts, and then on a regular basis to make sure red blood cell levels remain normal.
Who shouldn’t take testosterone replacement therapy?
Testosterone replacement therapy may cause the prostate to grow. If a man has early prostate cancer, there is concern that testosterone may stimulate the cancer’s growth. Therefore, men who have prostate cancer should not take testosterone replacement therapy. It is important for all men considering testosterone replacement therapy to undergo prostate screening before starting this therapy.
Other men who should not take testosterone replacement therapy include those who have:
- An enlarged prostate resulting in urinary symptoms (difficulty starting a urinary stream)
- A lump on their prostate that has not been evaluated
- A PSA measurement above 4
- Breast cancer
- An elevated hematocrit level (higher-than-normal number of red blood cells)
- Severe congestive heart failure
- Obstructive sleep apnea that has not been treated
Did you know?
- There is no evidence linking TRT to prostate cancer.
- There is no strong evidence linking TRT to increase in vein clots.
- At this time, there is no strong evidence that TRT either increases or decreases the risk of cardiovascular events. However, while you are on TRT, you should call your doctor right away if you have signs or symptoms of stroke or heart attack.






